At the 6th ASEAN International Integrative Oncology Medicine Session, Jim L. Fernandez, an oncology expert from Centro Escolar University in the Philippines, delivered a special report on Diagnosis, Prevention and Treatment of Oral Cancer. He systematically elaborated on the epidemiological characteristics, risk factors, diagnostic strategies, staging symptoms, treatment progress and prevention measures of oral cancer, and shared local clinical data from the Philippines, providing important reference for promoting oral cancer prevention and control in the Asia-Pacific region.

Oral cancer: a common tumor in the head and neck, with multiple risk factors that urgently need to be controlled.
Oral cancer is one of the most common types of head and neck cancers worldwide, primarily occurring in the oral cavity or oropharynx, with the tongue, lips, and floor of the mouth being particularly prevalent areas. Pathologically, over 90% of oral cancers are squamous cell carcinomas, and their malignancy and invasiveness have been confirmed by numerous regional studies. For example, in the Philippines, among 42 oral cancer patients treated at the Department of Otolaryngology-Head and Neck Surgery in Bicol Medical Center from 2018 to 2020, 38 patients (91%) were diagnosed with squamous cell carcinoma, and the majority of these tumors were in the advanced stages of IVA-IVB (76% in total), highlighting the urgent need to strengthen early screening for the disease.
Risk Factors and Prevention: Multidimensional Triggers and Proactive Interventions
During the forum, Dr. Fernandez detailed the main risk factors for oral cancer, covering three main categories: environmental exposure, infection, and lifestyle habits. These include smoking cigarette and cigar, human papillomavirus, EB virus, family history, poor oral hygiene, prolonged sun exposure, and chewing betel nut.
Regarding the diagnosis of oral cancer, Dr. Fernandez emphasized the importance of early identification and standardized assessment. He systematically introduced a series of diagnostic methods, including physical examination, brush biopsy, incisional biopsy, and indirect and direct laryngoscopy/pharyngoscopy, and provided a detailed analysis of the clinical manifestations of oral cancer at different stages: from early-stage leukoplakia, erythema, and non-healing ulcers, to mid-to-late-stage lymph node enlargement, speech impairment, dysphagia, and even distant metastasis. He cautioned, “Any oral ulcer or abnormal plaque that persists for more than two weeks should be taken very seriously.”

Dr. Fernandez emphasized the concept of “prevention is better than cure,” offering six core recommendations: quitting smoking and limiting alcohol consumption, sun protection and skin care, HPV vaccination, a balanced diet, maintaining good oral hygiene, and regular professional screening. He particularly urged that “people aged 20 to 40 should undergo oral cancer screening every three years, and those over 40 annually; this is a crucial step in preventing late-stage diagnosis.”
Diversified treatment methods: surgery is the primary approach, and integrated therapy being a trend
For treatment strategies, Dr. Fernandez points out that surgery is still the mainly treatment for oral cancer, with common procedures including primary tumor resection, glossectomy, mandibulectomy, neck dissection, and tissue reconstruction. Furthermore, sentinel lymph node biopsy is of significant value in determining whether cancer cells have spread. He emphasizes that modern oral cancer treatment has entered the era of integrative medicine. Compared to single-therapy approaches, integrative treatment, through multi-pronged synergy, can more comprehensively eliminate tumors, reduce the risk of recurrence and metastasis, and thus significantly improve patients' local control rates and long-term survival quality. In this regard, our hospital also adheres to the concept of “multidisciplinary integration,” customizing individualized comprehensive treatment plans for patients to strive for a balance between efficacy and quality of life.

Data from the Philippines reveals a grim reality: the high proportion of late-stage cases is drawing attention
As one of the countries with a high incidence of oral cancer in Southeast Asia, the Philippines' experience provides important lessons for regional prevention and control. Two clinical studies from Bicol Medical Center and Mariano Marcos Memorial Hospital show that oral cancer in the Philippines is characterized by high incidence, clustering of high-risk behaviors, late diagnosis, and low survival rates. The study from Bicol Medical Center, which published in the Philippine Journal of Otorhinolaryngology-Head and Neck Surgery, showed that between 2018 and 2020, 71% of oral cancer patients treated at the hospital were male, with an average age of 62 years. Squamous cell carcinoma accounted for 91%, with lesions mainly distributed in the anterior tongue and buccal region. More alarmingly, most patients were already at an advanced stage at the time of diagnosis, with stage IVA and IVB accounting for as high as 76%. Among patients with recorded risk factors, 61% had two or three high-risk habits simultaneously: betel nut chewing, smoking, and alcohol consumption, highlighting the importance of lifestyle interventions.
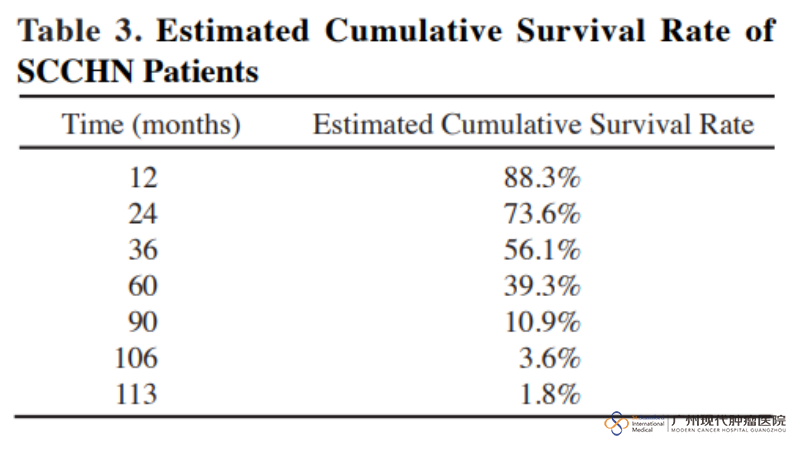
A retrospective study of 150 cases of head and neck squamous cell carcinoma at Mariano Marcos Memorial Hospital between 2003 and 2012 further revealed the profound impact of advanced disease on survival. The median age at initial diagnosis was 61.5 years, with a male-to-female ratio of 7:3, and 50.7% of cases had primary oral cancer. Although some patients underwent surgery or radiotherapy, overall survival significantly decreased with age compared to untreated patients. Data analysis showed no statistically significant association between treatment and patient survival, reflecting the difficulty of significantly improving prognosis with a single treatment modality in the context of advanced diagnosis. The study showed an overall mean survival of 49.3 months, with the survival rate plummeting from 88.3% in the first year to 1.80% at the end of the study, highlighting the poor prognosis of advanced oral cancer.
The two studies represent three key challenges in oral cancer prevention and control in the Philippines:
1. The high rate of late-stage diagnoses highlights the urgent need to improve screening and early detection capabilities;2. People with high-risk behaviors are highly concentrated, and public health urgently need to be strengthened;
3. Traditional treatments offer limited benefits to patients with advanced disease, which need to promote multidisciplinary collaboration and comprehensive management systems.
Promoting integrated healthcare to improve patients' quality of life and dignity
Based on the above research, Dr. Fernandez offered a clear vision for the future prevention and treatment of oral cancer. He emphasized the need to promote early screening and diagnosis to change the current situation where late-stage cases dominate. At the treatment level, he stressed the importance of developing and popularizing an integrative medicine model, which combines standardized surgery with radiotherapy, chemotherapy, and targeted therapy to create individualized comprehensive treatment plans for patients.
”Oral cancer is not only a medical issue, but also a public health issue,” Dr. Fernandez summarized. "We must work together on three levels—policy, healthcare, and public education—to promote early screening and diagnosis, popularize healthy lifestyles, and optimize treatment methods."
This forum, sharing by Dr. Fernandez, not only deepened participants’ understanding of the entire chain of oral cancer—from etiology to diagnosis, treatment, and prevention—but also highlighted the importance of multidisciplinary collaboration and regional experience exchange within an integrated medicine model. His advocacy of a “patient-centered, multidisciplinary integrated” treatment philosophy aligns perfectly with our hospital’s long-standing commitment to individualized and comprehensive treatment. Our hospital will continue to promote the deepening of the multidisciplinary team (MDT) model for cancer treatment, integrating cutting-edge technology with humanistic care, and is committed to not only treating diseases technically but also safeguarding the quality of every patient’s life and dignity through care.

*Surgery, in addition to the appropriate chemotherapy and radiotherapy, are effective in treating early cancer, but certain patients in late stage of cancer may not be tolerate surgery well as they can be relatively weak. A combination of carefully planned minimally invasive therapy, chemotherapy or radiotherapy can effectively reduce the side effects and discomfort of treatment and may help patient get better efficacy.













 viber
viber